What is Dysbiosis?
What is dysbiosis and what are the symptoms?
Simply put, the word ‘dysbiosis’ is the term given to an imbalance in the gut microbiome. We’re all becoming aware of the importance of good gut health, but how do you know when things are out of balance, and if so, what do you do about it? Read on to find out everything you need to know about gut dysbiosis, and how probiotics might help.
In this article we look at:
- What does a healthy gut microbiome look like?
- What causes dysbiosis
- Symptoms of dysbiosis
- How do I address dysbiosis?
- Summary
What does a healthy gut microbiome look like?
The short answer is that we are not yet sure, as no two microbiomes are the same. There is a huge degree of diversity from one individual to another, even in the absence of any obvious ill health or disease. In fact, it is thought that our microbiome is as unique to us as our fingerprint, which makes it difficult to categorise a microbiome as ‘healthy’ or otherwise. Often, they are just different.
Humans have trillions of bacteria and other microbes living within their digestive tract. These populations of microbes can be divided into three types: the ‘good guys’ (also known as probiotics) which offer benefits to their host, the ‘bad guys’ (pathogens), which can be harmful in large numbers, and ‘commensals’, which are benign, offering neither benefit nor harm to their host. The collective name for these colonies is the gut microbiome, and the health of the microbiome plays a surprisingly large role in our overall health and well-being. Find out more about the microbiome in Dr. Kate’s informative article.
It’s normal to have a mix of all three types of microbes in the gut, and even those with no obvious signs of ill health at all will still play host to pathogens. Pathogens may also include viruses, parasites, and yeasts, such as Candida albicans. Health professionals can read more about Candida overgrowth on the Professionals site.
However, as long as there are enough beneficial microbes to keep pathogen populations in check, they do not pose us any great problem. It is when there is a shift in the composition of the gut microbiome towards a higher proportion of pathogenic versus probiotic microbes that problems arise. This situation is referred to as ‘dysbiosis’.
Scientists have now identified many features that they think could be common to a healthy microbiome. These include:
1. The types of bacteria found in a healthy gut1
Two studies 2,3 have shown that healthy gut microbiomes (as assessed by bacterial gene sequencing) are consistently dominated by bacteria from two phyla (classes of bacteria): Bacteroidetes and Firmicutes. However, these phyla are huge, so it still leaves a multitude of different combinations of bacteria (belonging to these two groups) which could be considered a ‘healthy’ microbiome. (Read more about Firmicutes and their impact on our metabolism)
2. The number of different microbial ‘families’ inhabiting the gut2
It is widely accepted that the greater the diversity of probiotic microbes in the gut, the better. They have some common characteristics, like discouraging pathogens, but all probiotics fulfil slightly different functions. Therefore having a good variety of bacterial ‘families’ means that we might benefit from a broader spectrum of benefits.
3. Stable populations of microbes
It is generally accepted that a healthy gut microbiome is relatively stable. Reducing exposure to factors that can disrupt the delicate balance of gut microflora, such as antibiotics18, is essential to maintain this stable environment.
What causes dysbiosis?

Anything that shifts the health of the microbiome in such a way that it becomes less able to keep us healthy, is a factor for dysbiosis. Many external influences and lifestyle factors have a detrimental impact on the gut microbiome, including:
1. Antibiotics
Taking a course of antibiotics is well known to reduce the numbers of beneficial bacteria living in the gut, at the same time as reducing the pathogens that the drugs are being taken for. Whereas some species of friendly bacteria recover to some degree after antibiotic treatment ends, other species may be lost forever. The loss of friendly bacteria weakens the community’s future ability to exclude pathogens9 and prevent infections.
2. Certain medications
Certain medications are known to cause dysbiosis, by damaging the delicate gut lining and affecting the gut microbiome. Such medications include: NSAID’s, the contraceptive pill, HRT and steroid medications
3. High sugar diet
High sugar diet has been shown in studies to have a detrimental effect on the gut microbiota, by preferentially feeding yeasts and pathogenic species of bacteria, above beneficial strains of bacteria10. Additionally, a 2020 study discussed the possible negative effects of ‘novel’ or new types of sugars, such as chemically derived sweeteners and sugar alcohols on the gut flora. The study11 summarised that pathogens appear to have a greater ability to use and adapt to these new sugars than friendly bacteria species do. This could lead to further proliferation of ‘bad’ strains of bacteria in the gut, as we seek lower calorie, but often man-made alternatives to natural sugars.
4. Low fibre diets
Fibre is the preferred food source for many different strains of probiotic bacteria living in the gut. Our increasingly fibre-poor diets challenge the health of the microbiome, and one study showed that this has ‘lasting’ negative effects12.
5. Hormones
Our gut microbiota is sensitive to fluctuations in hormones, including the sex hormones, thyroid hormones and adrenal hormones. This is one reason why women suffer from gut-related symptoms such as constipation before their menstrual period, or during pregnancy.
6. Stress
Stress increases the levels of adrenal hormones circulating in the blood, and for this reason long-term stress is known to have a detrimental impact on various aspects of gut health. Research suggests that stress, and the impact of stress hormones, can make our gut ‘leaky’ or more permeable than it should be. Stress also alters immune activity in the gut and causes changes to the bacterial population that lives there13.
7. Age
Although not truly a lifestyle factor, our age can also have an impact on the microbiome. As the microbiome develops in an infants early years, we see significant changes. It then starts to stabilise before changing again significantly through pregnancy, menopause and as we enter old age. Read more about the microbiome in childhood years.
8. Foreign travel
When we travel we often come into contact with different microbes to those that we are used to, in both the local food and water. There are multiple pathogens that have been identified to be associated with Traveller’s Diarrhoea (TD), including: E coli, Shigella species, Campylobacter species and Norovirus14.
However, it is not only pathogens encountered in foreign destinations that can lead to dysbiosis when we travel. When we sleep may also be a factor. Doctors at the Weizmann Institute in Israel conducted fascinating research which showed that the activities of our gut bacteria follow a distinct circadian pattern. The research results showed that when the ‘host’ was asleep the microbiome was different to when the host was awake. This could explain why foreign travel, and the resulting change to our sleeping and eating times can greatly affect the microbiome, and cause digestive symptoms15.
What are the symptoms of dysbiosis?
When the gut microbiome is out of balance, symptoms of dysbiosis can arise. These symptoms may be felt principally in the digestive tract as digestive disturbances, but there may also be knock-on effects in other parts of the body, such as the immune system and organs of elimination, for example.
Probiotics produce beneficial metabolites, such as Vitamin K and short chain fatty acids, which can be used by the body, whereas pathogens produce toxins. When we have greater quantities of undesirable microbes in the gut, the organs of elimination (liver, kidneys, skin) must work harder to breakdown and then eliminate their toxins. Signs of poor detoxification can often be seen on the skin, with the appearance of skin conditions such as eczema, acne, psoriasis.
Emotional health may also suffer due to the impact of dysbiosis. ‘Psychobiotics’ is an area of science looking specifically at the impact of the gut microbiome on our mood and mental health. Many studies show a clear link between gut health and emotional health, and the microbiome is now known to play a significant role in our ability to synthesize certain hormones and neurotransmitters. Read more about the gut-brain axis and probiotics.
More recently links have been found between gut dysbiosis and certain metabolic conditions, including: Type 2 Diabetes, Metabolic syndrome and even obesity18. Inflammation caused by an imbalanced microbiota is thought to play a causative role in metabolic ‘dis-regulation’. In the case of obesity it has been observed that certain types of bacteria allow for a greater ‘harvest’ of energy from the foods that we eat, whilst also altering levels of available short-chain-fatty-acids in the gut. Read more about gut bacteria and obesity here.
Gut-related symptoms, include:
- Bloating
- Excess wind/flatulence
- Abdominal pain
- Diarrhoea
- Constipation
- Inflammatory Bowel Diseases16
- Irritable Bowel Syndrome17
- Acid reflux/GERD
- Halitosis
- Food intolerances/sensitivities
Other symptoms, include:
- Low mood/anxiety
- Difficulties sleeping
- Joint pain
- ‘Foggy’ thinking / poor concentration
- Skin complaints
- Sugar cravings
- Allergies16
- Metabolic syndrome16
- Obesity18
- Fatigue
How do I address dysbiosis?
So, how can we overcome dysbiosis, and recover from the myriad of possible symptoms that might arise as a result of it? You’ll be glad to hear that the solution is relatively straight-forward. We just need to nurture and feed our friendly bacteria.

Healing gut dysbiosis often requires a dual-pronged approach, as we need to work to eradicate the pathogenic over-growth, whilst encouraging the proliferation of healthy, probiotic microbes.
Let’s look first at how to eradicate the ‘bad guys’:
Stool testing
It can be useful to know which pathogens are present in your gut, and how many there are. Your GP can organise this for you, or if you prefer to take a more holistic approach to your wellbeing then you could work with a Nutritional Therapist or Medical Herbalist, who can also arrange a home-test kit for you. Read more about stool testing.
Antimicrobials
Dependent on your individual preferences, an effective anti-microbial protocol may involve either antibiotics from your GP, or nutritional/herbal remedies from a qualified natural health practitioner. There are many nutritional supplements with excellent anti-microbial properties, including: allicin (found in garlic), citricidal (found in grapefruit seed extract), oregano, colloidal silver, berberine (from grape seeds), olive leaf extract,
Diet
Eliminate certain foods from the diet which are known to preferentially feed pathogenic species of bacteria and yeasts, such as sugar11, sweeteners11 and refined carbohydrates.
Probiotics
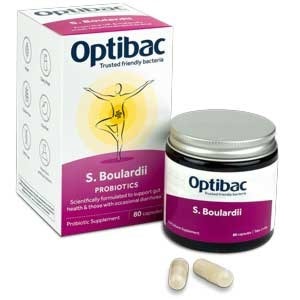
The probiotic yeast; Saccharomyces boulardii is one of the best probiotics for dysbiosis, and has demonstrated its anti-microbial effects in many clinical trials. It works in several ways, including preventing pathogens from adhering to the gut wall, and also binding their toxins17 You can find this strain in Optibac Saccharomyces boulardii.
Here’s how to nourish and nurture the ‘good guys’:
Fermented foods
Foods such as live yoghurt, kimchi, kombucha, sauerkraut, apple cider vinegar and kefir have been a part of traditional diets for hundreds of years. They contain naturally occurring probiotic bacteria, which support the microbiome.
Prebiotics
Include different sources of prebiotic fibre in your daily diet, by including a wide range of fresh fruit and vegetables, pulses and whole grains.
Probiotics
Take a well-researched, high-quality probiotic supplement every day. Different strains of probiotic bacteria produce acids and other by-products, which improve the intestinal environment, and favour the further growth of healthy species of bacteria. In this way we can ‘tip the balance’ back in favour of beneficial organisms and a healthier microbiota.
Several probiotic strains, including the strain Lactobacillus acidophilus NCFM ® have been studied and shown in clinical trials19 to help restore and stabilise the gut microbiota following antibiotic therapy.
You should always choose a probiotic supplement that has clinical research for your main symptoms. So, if bloating is your particular dysbiosis symptom, the best probiotics for dysbiosis in your case would contain strains that are well researched for bloating.
For those lucky few that do not show any signs of an unhappy gut, taking a high-quality probiotic every day still has great benefit, as it helps to prevent any future issues.
Summary
A lot has been covered in this blog, so here is a short summary of the main points:
- We rely on the health of the gut microbiome to keep us healthy.
- The microbiome always contains pathogens, but they are usually kept under control by the friendly strains of bacteria
- When there is a shift towards greater levels of pathogens and proportionately less probiotic bacteria this is known as dysbiosis
- Causes of intestinal dysbiosis include antibiotics, medications, stress, travel and poor diet
- Symptoms of dysbiosis, include gut-based symptoms, such as bloating and constipation, but also body-wide symptoms such as poor concentration, low immunity, and even metabolic syndrome.
- Correcting dysbiosis can be done by eradicating pathogens from the gut with either antibiotics, anti-microbial herbs/nutrients or the probiotic Saccharomyces boulardii. Coupled with replenishing the levels of friendly bacteria through improved diet and probiotic supplements.
Health Professionals can read more about Saccharomyces boulardii and Lactobacillus acidophilus NCFM ® over at the Probiotics Database).
References
- Shafquat A, et al. (2014 May). Review Functional and phylogenetic assembly of microbial communities in the human microbiome. Trends Microbiol. 22(5):261-6.
- Human Microbiome Project Consortium, (2012 Jun 13). Structure, function and diversity of the healthy human microbiome. J. Nature. 486(7402):207-14.
- Qin J et al, (2010 Mar 4). A human gut microbial gene catalogue established by metagenomic sequencing. J. Nature. 464(7285):59-65.
- Turnbaugh PJ, et al. (2009 Jan 22). A core gut microbiome in obese and lean twins. J. Nature. 457(7228):480-4.
- Turnbaugh PJ, et al. (2009 Sep 1). Review The core gut microbiome, energy balance and obesity. J. Physiol. 587(Pt 17):4153-8.
- Xu, Z et al. (2014 Dec.) Which is more important for classifying microbial communities: who's there or what they can do? ISME J. 8(12):2357-9.
- Abubucker S, et al. (2012). Metabolic reconstruction for metagenomic data and its application to the human microbiome. PLoS Comput Biol. 2; 8(6):e1002358.
- De Filippo C, et al. (2010 Aug 17). Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 107(33):14691-6.
- Dethlefsen L, et al. (2011). Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci U S A. 108 Suppl 1():4554-61.
- Sonnenburg ED, et al. (2016). Diet-induced extinctions in the gut microbiota compound over generations. J Nature. 529:212–5.
- Di Rienzi, S.C et al. (2020 May). Adaptation of the Gut Microbiota to Modern Dietary Sugars and Sweeteners. J. Advances in Nutrition. Volume 11, Issue 3. Pages 616–629.
- Sonnenburg ED, et al. (2014). Starving our microbial self: the deleterious consequences of a diet deficient in microbiota-accessible carbohydrates. J. Cell Metabol. 20:779–86.
- Karl JP, Hatch AM, Arcidiacono SM, et al. Effects of psychological, environmental and physical stressors on the gut microbiota. Front Microbiol. 2018;9:2013. doi:10.3389/fmicb.2018.02013.
- Youmans, BP. et al. (2015) Characterization of the human gut microbiome during travellers' diarrhoea. J. Gut Microbes; 6:110–9
- Thaiss, CA et al. (2014 Oct). Trans-kingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. J. Cell. 3;159(3):514-29. doi: 10.1016/j.cell.2014.09.048. Epub 2014 Oct 16.
- Carding, S. et al. (2015). Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis.; 26: 10.3402/mehd.v26.26191.
- Murzyn A, et al. (2010) ‘The effect of Saccharomyces boulardii on Candida albicans-infected human intestinal cell lines Caco-2 and Intestin 407’. FEMS Microbiology Letters 310 (1) 17-23.
- Fassarella M, Blaak EE, Penders J, et al. 2021. Gut microbiome stability and resilience: elucidating the response to perturbations in order to modulate gut health. J. Gut. 70:595-605
- Engelbrektson, A.L .et al., (2009). ‘Probiotics to minimize the disruption of faecal microbiota in healthy subjects undergoing antibiotic therapy’. Journal of Medical Microbiology, 58:663-670.
Popular Articles
View all Gut Health articles-
Gut Health04 Sep 2024
-
Gut Health28 Feb 2025
-
Gut Health02 Nov 2023