Natural remedies for IBS
Are you one of those 5 million desperately trying to find relief from IBS for good? Well look no further, you are in the right place. Hurrah!
The incidence of IBS (Irritable Bowel Syndrome) is rising dramatically worldwide, IBS now affects up to 14% of the global population1 and around 5 million adults in the U.K.2
The internet is completely awash with a vast array of IBS treatment options, so it’s no surprise that many sufferers find it overwhelming. Hopefully, by the end of this blog you will have a clearer understanding of IBS, the potential therapeutic role of probiotics, and will be armed with some simple tips.
Within this article:

What is IBS?
Irritable Bowel Syndrome or IBS is a common condition that affects the digestive system. It causes symptoms like stomach cramps, bloating, diarrhoea and constipation. The exact cause is unknown but sufferers report diet, lifestyle and environmental triggers. The diagnosis of IBS is given by a medical doctor once all other causes of these symptoms have been ruled out.
Is there a cure for IBS?
There are endless pages online suggesting various solutions including medications, supplements, herbal remedies and different diets. The thing is though, that not all IBS sufferers were created equal - we are all unique.
Conventional treatment focuses on symptom relief alone, but it is important to identify the underlying cause, and the causes and triggers of IBS can vary greatly. But, IBS is certainly not something you have to live with, and by using a combination of three well researched methods, you could become symptom-free for good.
3 steps to IBS relief
The following recommendations are based on the classic 4R protocol favoured by health care practitioners like Nutritional Therapists. They will enable you to understand your body, determine your triggers, and keep your gut happy.
1. Dietary Triggers
Eating certain foods can cause significant digestive symptoms to those with IBS4, the most common dietary triggers are gluten (in many foods, not just bread), cow’s milk, eggs, caffeine, and alcohol. But perhaps the most common triggers are foods that come under an umbrella term called ‘FODMAP’ foods, like garlic and onions.

What are FODMAPs?
FODMAP stands for "Fermentable Oligo-, Di-, Mono-saccharides And Polyols". These carbohydrate-rich foods are often poorly digested in the small intestine and cause gas, bloating and changes in stool pattern.
High FODMAP foods:
- Wheat
- Dairy
- Onion
- Garlic
If you notice you have IBS symptoms after eating a certain type or food, or if it’s worse in the morning or night-time, then start keeping a record (use your phone if you’re out and about) of what you have eaten that day. If you start to see a pattern occurring, you could be intolerant or sensitive to those foods.
If you spot a pattern, you may want to try temporarily remove the food item in question from your diet for a few weeks to see if your symptoms improve. If your triggers seem to be FODMAP foods, then following the low-FODMAP diet can be beneficial, but do note that this diet should not be followed for more than a month, as many of these foods are great for feeding good bacteria so you do not want to withhold these from your diet for any extended period. Ideally, the FODMAP diet should only be embarked upon with the advice and guidance of a qualified health practitioner.
2. Probiotics
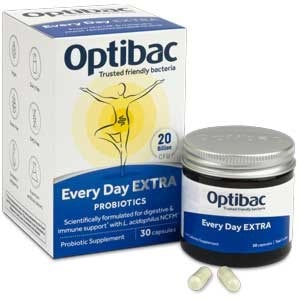
As IBS is a condition affecting the gut and digestive health, it makes sense to consider supporting gut health and the microbiome as part of your IBS health regime. Learn more about the microbiome by reading: All About The Microbiome. Probiotics have been shown in studies to significantly reduce the symptoms of IBS5, but it’s important to point out that not all probiotics act in the same way. Picking the best probiotic strains for IBS depends on the clinical research which supports them - find out why exact probiotic strain matters.
The worlds most clinically researched strain of Lactobacillus acidophilus with over 60 clinical trials behind it is L. acidophilus NCFM®. This strain has shown to lower symptom severity of IBS complaints, particularly abdominal cramping and bloating where 73% of participants reported less bloating in as little as 4 weeks.
Not only has this strain demonstrated impressive results for reducing symptoms, it can also help with one of the most common food intolerances: dairy. It can aid in the digestion of lactose as Lactobacillus bacteria possess lactase activity (the enzyme needed to break down lactose).
Another strain that has been especially researched for IBS is Lactobacillus plantarum LP299v®. This strain has shown in studies to be particularly good at lowering pain and bloating scores in those with IBS. With the pain of IBS often described as “like being in labour”, any reduction has got to be a good thing, right?
To find out more about the different probiotic strains which have been researched for IBS symptoms, see our article: Which probiotics for IBS?
So how long do you take probiotics for IBS?
To allow time for the microbiome to rebalance, it is recommended to take probiotics for at least 2-3 months, but many IBS sufferers choose to take probiotic supplements on an ongoing basis.
3. Lifestyle factors affecting IBS
Are you feeling frazzled and stressed out from ALL the pressures of modern day living? It is worth considering if stress triggers your IBS symptoms.

Stress puts us into the ‘fight or flight’ state and can alter digestive function. In short, our blood gets sent to our limbs and brain (to run away from a perceived threat) and digestion of food gets put on the back burner.
Bloating and constipation are undesirable side effects resulting from this type of stress. There's a definite interplay between the two, where stress can cause bloating and vice versa. Learn more about the relationship between stress and bloating.
Following these simple tips can help you relax before meals; this will give your body the best chance of being able to break down and digest your food properly.
- Sit down to eat in a quiet and comfortable place, with no screens.
- Take three full, deep belly breaths before you start eating.
- Chew your food properly, aim for a minimum of 15 chews per mouthful.
Anxiety provokes IBS and IBS provokes anxiety; thus ensues a vicious cycle that can be hard to break. The link between the gut and the brain (the so-called gut-brain axis) has been extensively researched and studies continue to take place in this area. Learn more about the gut-brain axis.
Breaking this cycle can be challenging, but not impossible.
Taking up a meditation practice is not only good for helping you deal with stress and anxiety, but it has shown to improve pain and bloating scores in up to 57% of participants with IBS in one study6.
Why not give it a go?
Summary: your easy IBS action plan
- Keep a food & symptom diary to identify triggers
- Take a good quality probiotic supplement
- Try mindful eating and daily meditation
Final thoughts
If you are unsure whether you have IBS or not, you should always discuss your symptoms with your GP first so you can get a diagnosis. It’s important to rule out any other more serious issues like IBD (Crohn’s disease, ulcerative colitis and diverticulitis), ovarian cancer, endometriosis and coeliac disease.
If these tips don’t help, you may have a more complex underlying cause, in which case it would be worth seeking the advice of a qualified health professional like a Nutritional Therapist. For the unlucky few, there may be a need to undergo a comprehensive stool analysis with the help of a qualified healthcare practitioner to determine the underlying cause of IBS, which could be a parasite residing in the gut. Parasites can be picked up from travelling to exotic destinations or eating raw or uncooked food.3 You may like to learn more about gut microbiome tests here.
But the majority of IBS sufferers can do lots to help themselves with simple, safe, natural methods and supplements.
Want to read more?
Gut Health - All You Need to Know
Probiotics for Bloating
Health care professionals can read more about the strains in this article on the Probiotics Database.
Healthcare professionals can read more about lactose intolerance and probiotics on the Probiotics Professionals site.
References
- Monia E. Werlang, William C. Palmer, and Brian E. Lacy (2019). Irritable Bowel Syndrome and Dietary Interventions. Gastroenterology & Hepatology. 1 (1), 16-19.
- NICE. (April 2017). Irritable bowel syndrome in adults: diagnosis and management. Available: https://www.nice.org.uk/guidance/cg61/chapter/introduction. Last accessed 06/11/2019.
- Maria Elena Ramirez-Miranda, Rosaura Hernandez-Castellanos, Eduardo Lopez-Escamilla, David Moncada, Alfredo Rodriguez-Magallan, Carlos Pagaza-Melero, Alberto Gonzalez-Angulo, Ana Flisser, Simon Kawa-K. (2010). Parasites in Mexican patients with irritable bowel syndrome: a case-control study. Parasites & Vectors. 1 (3), 96.
- Shanahan, F. and P.J. Whorwell, M.D. (2005). IgG-mediated food intolerance in irritable bowel syndrome: A real phenomenon or an epiphenomenon? The American Journal of Gastroenterology. 100:1558–1559.
- Williams EA1, Stimpson J, Wang D, Plummer S, Garaiova I, Barker ME, Corfe BM.. (2009). Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study.. Alimentary pharmacology and therapeutics. 29 (1), 97-103.
- L. Keefer , E.B. Blanchard. (2002). A one-year follow-up of relaxation response meditation as a treatment for irritable bowel syndrome. Behaviour Research and Therapy. 40 (3), 541–546.
Popular Articles
View all Gut Health articles-
Gut Health27 Nov 2023
-
Gut Health15 Nov 2023


