Probiotics and Lyme Disease
Within this article we discuss:
- What is Lyme disease?
- Symptoms
- Can probiotics help?
- Probiotics alongside antibiotics treatment
- Yeast overgrowth and Intestinal permeability
- Immune support
- Inflammation
- Gastrointestinal symptoms
- Conclusion
What is Lyme disease?
Lyme disease is a bacterial infection spread to humans by bites from infected ticks. Within days of being bitten by an infected tick, in some cases, a circular rash which is known as ‘erythema migrans’ will form at the site of the bite.
Lyme disease is caused by a bacteria known as Borrelia burgdorferi. Researchers from the ‘Centers for Disease Control and Prevention’ (CDC) have recently identified another species known as Borrelia mayonii – closely related to Borrelia burgdorferi – which is also thought to cause Lyme disease 1,2.
According to the NHS, within the UK, there are 2000-3000 new cases of Lyme disease each year, and 15% of these cases occur whilst the affected individuals are abroad 3. Getting a definitive diagnosis of this condition can prove to be quite difficult in some cases. A survey carried out by Caudwell Lyme Disease charity involving 500 Lyme disease patients found that 69% of the participants had actually been suffering from Lyme disease for over two years before the diagnosis was confirmed 4.

Symptoms
Initially, infected individuals may experience flu-like symptoms, fever, headache, fatigue, and body aches. If not treated promptly, sufferers may go on to develop more serious symptoms like Lyme carditis (heart palpitations), inflammatory arthritis and inflammation of the brain and spinal cord as a result of meningitis5. In some cases, problems with the nervous system may occur, such as paralysis of the facial muscles (facial palsy), memory problems, and difficulty concentrating6.
Can probiotics help?
There’s currently not a lot of research that specifically looks at the use and effects of probiotics for Lyme disease, but there’s growing interest in their use amongst sufferers. So let’s think about how probiotics might be helping these individuals both during treatment and for symptom support.
Probiotics alongside antibiotics treatment
As soon as Lyme disease is identified, individuals are usually given a 2-week course of antibiotics, but where more severe symptoms are present, the antibiotic course could last for up to 4 weeks and intravenous antibiotics treatment might be necessary for some.
I always say there’s a place for antibiotic treatment and when it comes to Lyme disease, this medication could be lifesaving. It’s very important that individuals are able to complete the course of antibiotics to ensure that the bacterial infection is eliminated completely; however, some individuals find it difficult to complete their course of antibiotics due to the side effects that often accompany this type of medication. Common side effects associated with antibiotics include thrush, diarrhoea, loss of appetite and abdominal pain, but some antibiotics used to treat Lyme disease could also cause sensitivity to sunlight! Learn more by reading: Which probiotics help with thrush?
Now here is a very specific area where probiotics could offer some support to sufferers of Lyme disease. Taking live cultures could help to reduce the risk of unpleasant side effects, enabling individuals to complete their antibiotic course and reduce the risk of issues like antibiotic resistance7. See our FAQ in the Probiotics Learning Lab for more information about this: Can I take live cultures with antibiotics?
Head over to Learning Lab and take a look at Dr Aisling's blog for more information on why to consider probiotics with antibiotics.
Some individuals find it difficult to complete their course of antibiotics due to the side effects
Yeast overgrowth and Intestinal permeability
But though antibiotic medication is a crucial part of the treatment for Lyme disease, there can be some lasting after-effects resulting from the use of this medication. Dr. Nicole McFadzean talks about the downsides of using long-term antibiotic supplements for individuals struggling with chronic Lyme disease8. She explains:
“The two major drawbacks of this approach are (1) the “Herxheimer reaction”, which is a detox-type reaction that may occur during initial phases of treatment. As the spirochetes are killed off and expelled from the body, they can create a worsening of symptoms. (2) The side effects of the medications. One of the most notable secondary effects of such longer term antibiotic regimens is yeast overgrowth in the gut. Preventive measures must be taken to minimize the chance of this.”
The role of antibiotics in the pathogenesis of yeast overgrowth has been researched over the years and a number of studies have found a significant association between antibiotic treatment and the onset of yeast infections like Candida9,10.
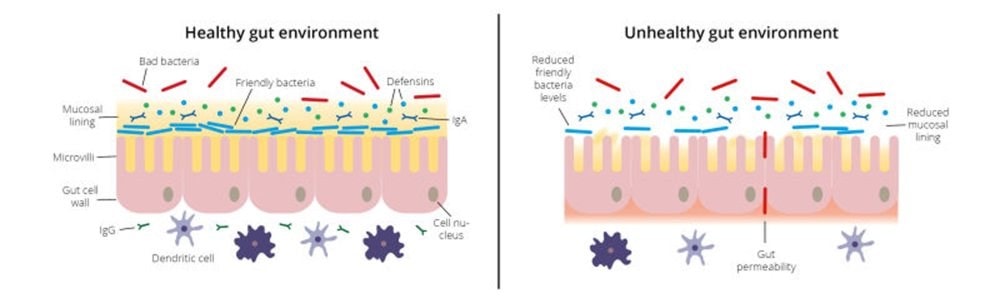
As I mentioned earlier, antibiotic treatment can be very vital in the treatment; however, as well as killing the pathogenic bacteria, the medication can also wipe out some of our friendly bacteria as well, which could lead to intestinal dysbiosis. Intestinal dysbiosis could potentially lead to intestinal permeability (leaky gut) and Candida overgrowth can also lead to the loosening of the tight junctions adjoining epithelial cells.
Saccharomyces boulardii, which is a probiotic yeast, has been shown to inhibit pathogenic microorganisms like Candida yeasts from attaching to the intestinal wall11. Supplementing with probiotics and replenishing the good bacteria in the gut also encourages other helpful species to flourish.
You can find Saccharomyces boulardii in Optibac Probiotics Saccharomyces Boulardii.
Learn more about the research behind Saccharomyces boulardii on the Probiotics Database.

Immune support
Some individuals with Lyme disease could develop long-term symptoms, collectively known as ‘Post-infectious Lyme disease’, which can manifest and continue long after the infection has been identified and treated 6. These individuals experience symptoms like joint and muscle aches, fatigue, and other symptoms similar to chronic fatigue syndrome (CFS). Sadly, it’s not clear why this happens and why it only affects some of the people who contract the infection; however, it is believed that it’s not caused by persistent infections, but instead by possible damage to tissues and over-activity of the immune system during the initial infection6,14.
As well as transferring the bacteria that causes Lyme disease, ticks can carry and transfer other bacteria, viruses, and parasites in the same bite, which could lead to multiple infections (co-infection)15. Co-infections could cause worse presentation of symptoms and affect the success of treatments.
Because Lyme disease is caused by a bacterial infection, the way the body reacts to this is important. During a typical infection, our body’s immune system jumps in and initiates a set of immune responses to help fight off and eliminate the invading pathogens. However, if the immune system is weak, then our ability to protect ourselves against these invading pathogens is compromised.
So it’s important to ensure we support our immune system to reduce the risk of infection. Our intestinal microflora, immune and nervous system interact quite closely together, and it's believed that the effectiveness of this interaction between our intestinal immune system and gut microbiota could very well predict the outcome of health and disease16.
This is another area where probiotics may offer additional support. As practitioners, you’re probably very familiar with the fact that 70% of our immune cells reside within our gut. So when it comes to Lyme disease, in theory, supporting your patient's immune function could be a key area of focus to help them overcome the infection more effectively.
The gastrointestinal tract is coated with a myriad of different friendly bacteria which all provide a barrier against incoming pathogens, but some types of bacteria seem to show more potential than others for immune support. Strains like Lactobacillus paracasei CASEI 431® have been shown to inhibit the growth of many pathogens by increasing the integrity of the gastrointestinal tract and stimulating the secretion of molecules like bacteriocins and defencins which inhibit the growth of pathogenic bacteria and yeasts in the gut.
You can find Lactobacillus paracasei CASEI 431® in Optibac Probiotics Immune Support.
Read more about the research behind Lactobacillus paracasei CASEI 431® on the Probiotics Database.
Inflammation
A lot of symptoms experienced by Lyme disease sufferers could also be caused by inflammation. Inflammation is one of the body's natural defences so it’s not necessarily a bad thing; however, prolonged and chronic inflammation - like those observed in some Lyme disease cases long after diagnosis and treatment - can be quite detrimental to the body and could cause systemic inflammation which could lead to autoimmune conditions like arthritis5.
The microbiota can detect pathogenic microorganisms and stimulate the immune system to mount appropriate responses12. The exact mechanism by which the microbiota triggers anti-inflammatory responses is not clear; but, probiotics are thought to prevent inflammation by increasing the integrity of the gut wall lining, and displacing pathogens which may trigger pro-inflammatory responses from the immune system. Beneficial bacteria are believed to promote the production of anti-inflammatory mediators.
Bacterial strains like Lactobacillus acidophilus NCFM®, Bifidobacteria lactis Bi-07® and Bifidobacteria lactis Bl-04® have been researched to help determine their role in supporting immune function, inflammation, improving antibiotics side effects and balancing the gut flora13.
Find out more about Lactobacillus acidophilus NCFM®, Bifidobacteria lactis Bi-07® and Bifidobacteria lactis Bl-04® on the Probiotics Database.
Gastrointestinal symptoms
Lyme disease can cause some uncomfortable gastrointestinal symptoms like diarrhoea, nausea and abdominal pain in some cases17. These symptoms can be quite debilitating for Lyme disease sufferers and in some cases, it has been associated with the onset of issues like panic attacks, depression, anorexia, and dementia!6,18
There are a number of well researched bacterial strains that have been found to be quite helpful at managing gastrointestinal symptoms like diarrhoea, bloating and IBS type abdominal discomfort. Saccharomyces boulardii has been found in a number of studies to reduce diarrhoea symptoms and even antibiotic-associated diarrhoea. Some strains within the Lactobacilli and Bifidobacteria genera have also been shown to be helpful in managing symptoms like bloating, gas and abdominal cramps 19, 20.
Conclusion
To conclude, whilst there aren’t many studies specifically focusing on a role for probiotics in the support of Lyme disease, it’s worth remembering that potentially, there are a few ways in which probiotics could prove to be of benefit for sufferers in the management of the condition. So as practitioners, it’s worth ensuring that our clients' guts are not forgotten, both during the treatment and recovery process. I call the gut flora the unsung heroes of our bodies as they’re often pushed aside in some cases where they’re literally dying to help!
Trust us to keep you posted about the latest research when it comes to probiotics, so watch this space for more updates on probiotics and Lyme disease.
In the meantime, check out the following links for more interesting research:
Probiotics and Leaky Gut, a look at the research
Probiotics Database - Immunity
And see these articles in the Probiotics Learning Lab:
The Antibiotics Myth
Study suggests Chronic Fatigue syndrome may be linked to imbalance in gut bacteria
References
- Centers for Disease Control and Prevention (CDC), 2017. Centers for Disease Control and Prevention. [Online]. Available at: https://www.cdc.gov/lyme/postlds/index.html. [Accessed 16 November 2017].
- Steere, A. C., Coburn, J. & Glickstein, L., 2004. The emergence of Lyme disease. Journal of Clinical Investigation, 113(8), pp. 1093-1101.
- Beasley, D., 2017. Huff Post. [Online]. Available at: https://www.huffingtonpost.com/entry/scientists-discover-new-bacteria-responsible-for-lyme-disease_us_56ba2000e4b08ffac122b719. [Accessed 03 November 2017].
- Caudwell Lyme Disease charity, 2016. Lyme disease UK. [Online]. Available at: http://lymediseaseuk.com/wp-content/uploads/2016/11/lyme-disease-on-the-nhs-ppt-v1.pdf. [Accessed 28 November 2017].
- Pachner, A. R., 1995. Early disseminated Lyme disease: Lyme meningitis. The American Journal of Medicine, 98(4), pp. 30S-43S.
- Stricker, R. B. & Fesler, M. C., 2017. Chronic Lyme Disease: A Working Case Definition. Chronic Dis Int, 4(1), pp. 1-10.
- Surkov, A., 2014. Role of probiotics in prevention and treatment of antibiotic-associated diarrhea in children. Pediatric pharmacology, 41(11), p. 41.
- Nicola McFadzean, N., n.d. Restor medicine. [Online]. Available at: https://restormedicine.com/lyme-disease-a-cause-of-fibromyalgia-chronic-fatigue-and-arthritis/. [Accessed 09 February 2018].
- Marie , P. V. & Garland, S. M., 2006. Genital Candida Species Detected in Samples from Women in Melbourne, Australia, before and after Treatment with Antibiotics. Journal of Clinical Microbiology, 44(9), pp. 3213-3217.
- Mayer, F. L., Wilson, D. & Hube, B., 2013. Candida albicans pathogenicity mechanisms. Landes Bioscience, pp. 119-128.
- Murzyn, A. et al., 2010. Capric Acid Secreted by S. boulardii Inhibits C. albicans Filamentous Growth, Adhesion and Biofilm Formation. 5(8), p. e12020.
- Vitetta, L. et al., 2012. A review of the pharmacobiotic regulation of gastrointestinal inflammation by probiotics, commensal bacteria and prebiotics. Inflammopharmacology, 20(5), pp. 251-266.
- Lomax, A. R. & Calder, P. C., 2009. Probiotics, Immune Function, Infection and Inflammation: A Review of the Evidence from Studies Conducted in Humans. Current Pharmaceutical Design, 15(13), p. 1428.7.
- NHS Choices, 2015. NHS Choices. [Online]. Available at: https://www.nhs.uk/conditions/lyme-disease/. [Accessed 9 November 2017].
- Berghoff, W., 2012. Chronic Lyme Disease and Co-infections: Differential Diagnosis. The Open Neurology Journal, 6(1), pp. 158-178
- Mariño, E., 2016. The gut microbiota and immune-regulation: the fate of health and disease. Clinical & Translational Immunology, 5(11), pp. 1-2.
- Feder, H. M. et al., 2007. A Critical Appraisal of “Chronic Lyme Disease”. New England Journal of Medicine, 357(10), pp. 1422-1430.
- Fallon, B. A. & Nields, J. A., 1994. Lyme disease: a neuropsychiatric illness. The American Journal of Psychiatry, 151(11), pp. 1571-1583.
- Ringel-Kulka, T. et al., 2011. Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: a double-blind study.. Journal of Clinical Gastroenterology, 45(6), pp. 518-525.
- Faber, S. M., 2000. Treatment of abnormal gut flora improves symptoms in patients with irritable bowel syndrome. The American Journal of Gastroenterology, 95(9), p. 2533.
Popular Articles
View all General Health articles-
General Health17 Mar 2023


