Probiotics and PCOS
Polycystic ovary syndrome (PCOS) is a common endocrine condition affecting 5-10% of women1,2 It is estimated that over 3 million women in the UK have PCOS. In this article we delve into this condition, and explore the research into probiotics for PCOS.
What is PCOS?
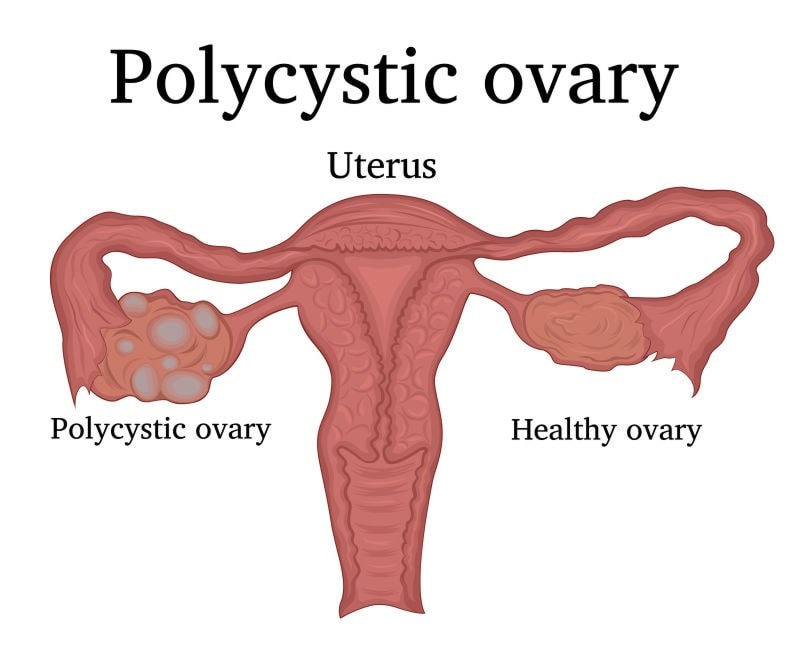
PCOS affects how the ovaries work and it’s characterised by a number of features. One of them being the formation of small underdeveloped cysts in the ovaries, known as cyctic ovaries, which can affect the menstrual cycle as some of the sacs can’t release an egg, impeding ovulation3.
Another feature of PCOS is an imbalance in sex hormones, so excess androgens are produced by the ovaries and released into the body. Although androgens are normal residents in a woman’s body as they’re converted into oestrogen, high levels are linked to PCOS and other health issues4.

Causes of PCOS
PCOS is a complex condition, with no known cause or cure and it isn’t thought to be hereditary; however, it’s often linked to raised inflammation and high levels of hormones like insulin. Often, women with PCOS develop insulin resistance as their bodies become resistant to the effect of insulin, which leads to more insulin being secreted by the pancreas.
This can contribute to a number of serious health issues like type 2 diabetes, obesity, and overproduction of testosterone which can affect ovulation3. Sadly, for many women it becomes a negative health cycle.
Whilst there is no cure for PCOS, there are a number of options available that could help with improving individual symptoms some women struggle with. Lifestyle and dietary interventions like dietary management, exercise and losing excess weight can help with improving some symptoms.
It is well known that probiotic bacteria protect cells in the digestive system by forming a thick, protective barrier to stop pathogens from attacking. A compromised gut barrier, known as leaky gut, allows toxins and pathogens through, triggering immune cells to respond by increasing inflammation, one of the hallmarks of PCOS.
There are a number of natural remedies that may offer support for symptoms of PCOS. One example is a prebiotic supplement, which could help promote the growth of beneficial bacteria in the gut that are involved in the metabolism of carbohydrates.

PCOS and the gut microbiome
A theory by Tremellen & Pearce (2012) looked at dysbiosis of the gut microbiota (DOGMA), as a possible answer to the aetiology of PCOS5. Their theory suggested that intestinal dysbiosis caused by poor diet could increase intestinal permeability which could lead to lipopolysaccharides (LPS) escaping into circulation in the body. LPS are found on the outer layer of gram negative bacteria, which can stimulate strong immune response. This immune response could lead to a cascade of events that could affect insulin levels, production of androgen and consequently the ovaries.
Guo, et al. (2016) built on this hypothesis and carried out a murine study based on the DOGMA theory6 . The study involved 32 female rats, split into 4 groups of 8. They found that Lactobacillius, Ruminococus and Clostridium were lower in the PCOS rats compared to the control. These rats also had higher Prevotella species compared to the other controls.
One PCOS group were monitored and were given faecal microbiota transplants (FMT), another PCOS group had Lactobacillus transplantation. Both groups displayed a high amount of Lactobacillus and Clostridium similar to the healthy control groups, days after the treatments. The PCOS groups that had the FMT and the transplant treatment, had an improved estrous (reproductive) cycle after the treatments. They also found that the androgen and testosterone concentration in the treated rats decreased significantly compared to the control group.
This result further demonstrate that there could be a link between the gut flora and PCOS. More recently, a 2022 review reported women with PCOS as having less diverse and beneficial gut bacteria10 and possibly more likely to suffer with IBS.
Probiotics for PCOS
As practitioners, I’m sure you’re wondering about probiotics for PCOS - how probiotics can help with managing PCOS. Well, let's take a look at a the latest research studies.
A number of studies have found that supplementing with probiotics could have positive effects on some of the issues associated with PCOS9 like insulin sensitivity, inflammation and LPS production; so, supplementing with probiotics could very well help with factors associated with PCOS.
A randomised double blinded placebo study, assessed the effect of Lactobacillus acidophilus NCFM® on insulin sensitivity and systemic inflammation in male volunteers7. The study involved 43 male volunteers. They were split into two groups, each group including men diagnosed with type 2 diabetes and some with normal glucose tolerance. One group received Lactobacillus acidophilus NCFM® and the other group were given a placebo over a period of 4 weeks. Although there were no significant improvements in systemic inflammation in both groups, insulin sensitivity in the group that received the probiotic supplement improved.
This clinical trial highlights the possible role probiotics could play in supporting insulin sensitivity which is often an issue with PCOS. So, whilst this trial was carried out on men, the positive result might suggest that it could also be applicable to women with insulin sensitivity.
Another murine study also explored the effect probiotic supplementation has on reducing the production of LPS8. They found that Lactobacillus rhamnosus GR-1® significantly decreased the production of LPS-induced production of interleukin - known to stimulate immune responses like inflammation.
It is thought that women with PCOS tend to have lower levels of Lactobacillus in their vaginal microbiome than women without PCOS. Ideally, Lactobacillus should be the dominant bacteria in the vagina. Therefore, probiotic strains which target the vaginal microbiome, such as Lactobacillus rhamnosus GR-1, Lactobacillus reuteri RC-14 and Lactobacillus paracasei F-19, may be helpful for women with PCOS.
Key takeaways
Compared to women without PCOS, research shows us that those with PCOS tend to have differences in the gut microbiome:
- A less diverse microbiome
- Lower levels of Bifidobacteria
- Less bacteria that produce SCFA's (short chain fatty acids)
- More pathogenic microbes like Streptococcus spp. and E. coli
All in all, although the research into the effect the microbiota has on PCOS is quite promising, due to the complexity of pathogenesis of this condition, more human clinical trials will need to be carried out to further explore how probiotics for PCOS can be used in practice.
Check out the following links for more research involving probiotics;
Do probiotics help curb inflammation and obesity?
Probiotics and Leaky Gut, a look at the research
References
- B. O. Saydam and B. o. Yildiz, "Gut-Brain Axis and Metanolism in Polycystic Ovary Syndrome," Current Pharmaceutical Design, vol. 22, no. 36, p. 5572, 2017.
- PCOS UK, "PCOS UK," 2013. [Online]. Available: http://www.pcos-uk.org.uk/about-pcos.html. [Accessed 22 September 2017].
- NHS, "NHS Choices," NHS, 18 03 2016. [Online]. Available: http://www.nhs.uk/conditions/polycystic-ovarian-syndrome/Pages/Introduction.aspx. [Accessed 22 September 2017].
- M. C. N. I. F. Dr. James Simon, "Healthy Women," 2017. [Online]. Available: http://www.healthywomen.org/condition/androgen. [Accessed 22 September 2017].
- K. Tremellen and K. Pearce, "Dysbiosis of Gut Microbiota (DOGMA) – A novel theory for the development of Polycystic Ovarian Syndrome," vol. 79, no. 1, p. 104, 2012.
- Y. Guo, Y. Qi, X. Yang, L. Zhao, S. Wen, Y. Liu and L. Tang, "Association between Polycystic Ovary Syndrome and Gut Microbiota," Journal pone, vol. 11, no. 4, pp. 1-15, 2016.
- A. S. Andreasen, N. Larsen, T. Pedersen-Skovsgaard, R. M. G. Berg, K. Møller, K. D. Svendsen, M. Jakobsen and B. K. Pedersen, "Effects of Lactobacillus acidophilus NCFM on insulin sensitivity and the systemic inflammatory response in human subjects," British Journal of Nutrition, vol. 104, no. 12, pp. 1831-1838, 2010.
- S. Yang, W. Li, . J. R. Challis, . G. Reid, S. O. Kim and A. D. Bocking, "Probiotic Lactobacillus rhamnosus GR-1 supernatant prevents lipopolysaccharide-induced preterm birth and reduces inflammation in pregnant CD-1 mice," vol. 211, no. 1, p. 44, 2014.
- Arab A et al., (2022) Effects of probiotic supplementation on hormonal and clinical outcomes of women diagnosed with polycystic ovary syndrome: A double-blind, randomized, placebo-controlled clinical trial. Journal of Functional Foods, 96:105203.
- Gu Y. et al., (2022) Gut and Vaginal Microbiomes in PCOS: Implications for Women’s Health. Frontiers in Endocrinology, 13: 808508. doi: 10.3389/fendo.2022.808508