Effects of Crohn's Treatments on Gut Flora
Inflammation underpins many chronic health conditions, and so trying to modulate inflammatory responses is an issue that occupies the minds of medical doctors, researchers and natural therapists alike. Crohn’s disease is one such condition, and it can be a constant battle to try and minimise the unpleasant symptoms that can present in this difficult health complaint. The role of the microbiome in Crohn’s is becoming widely-recognised, and a new study has looked at the current treatment options for the disease, and how these affect the delicate gut flora in sufferers.
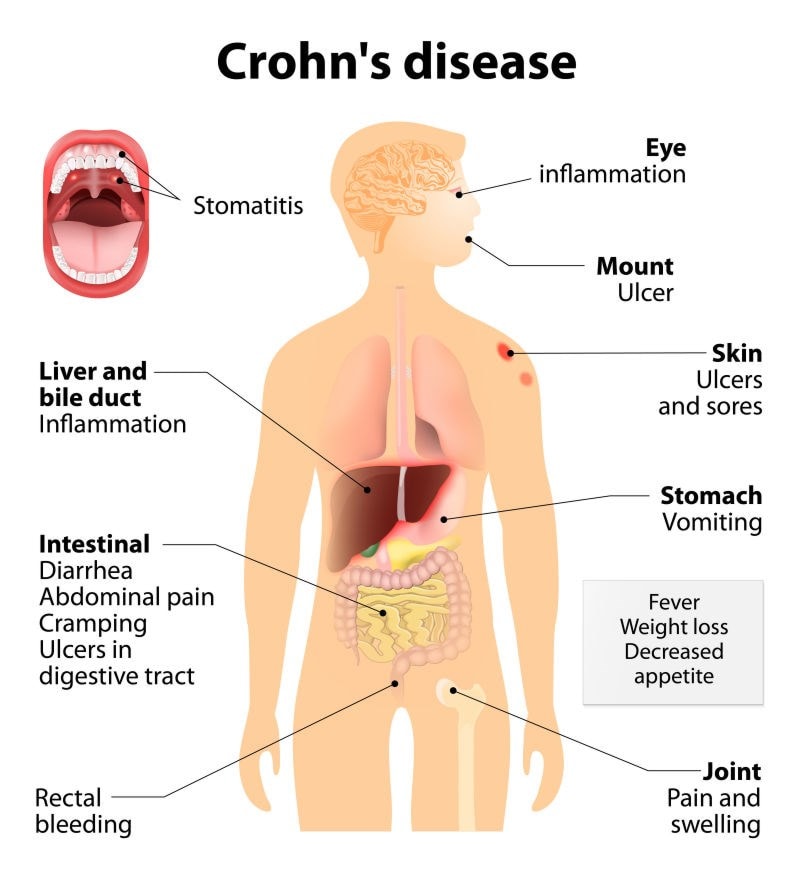
The study, which was published in Cell Host and Microbiome and conducted by researchers from the Perelman School of Medicine at the University of Pennsylvania, first analysed stool samples obtained from 90 children suffering from Crohn’s disease and 26 healthy child control subjects. They recorded the levels of bacteria, fungi, archaea, and viruses that were present in the children’s intestines, and then monitored how these populations were affected by different types of Crohn’s treatment. Enteral nutrition and levels of anti TNFa antibodies were also monitored.

Antiobiotics were shown to suppress the growth of bacteria, but provided conditions ripe for fungal overgrowth. Specially modified diets did help to reduce inflammation and resulting in an alleviation of symptoms, but did not have a positive effect on the balance of intestinal flora. Anti-inflammatory treatments did affect the composition of the gut microbiome, but did not effectively restore a desirable balance of flora.Treatment with immune-suppressants did positively affect both inflammation and generalised bacterial imbalance, but again, these treatments still allowed yeasts to proliferate.
“The formula based diet helped the children to improve their symptoms and inflammation despite making the microbiota initially more dysbiotic,” said co-senior author Gary Wu, MD, a professor of Gastroenterology. “This is an intriguing finding implying that it may not be necessary to completely restore a healthy microbiome to provide a beneficial effect.”
Removing problem foods from the diet can help to rest a compromised digestive system, but is not always a solution in itself; could it be possible in the future to provide a combination therapy that helped to relieve symptoms but also rebalance the intestinal flora?
Another case for 'Personalised Microbial Intervention?'
The study did appear to confirm that intestinal dysbiosis is a major factor in the development of Crohn’s disease, but that each patient may well require individualised programmes for treatment and recovery. In my recent blog about Personalised Microbial Intervention, which you can read over in the Probiotics Learning Lab, I touched on the fascinating subject of the potential for a ‘tailor-made’ probiotic supplement; as experts in ‘strain specificity’, this area of research is one which is of particular interest to us.
Is this further proof of the ‘one microbiome does not fit all?’ ethos that is beginning to prevail in the arena of probiotic research? Also, perhaps, more fodder to support the ‘Hygiene Hypothesis’? Is Crohn’s an autoimmune disease that ultimately results from being ‘too clean’? Do some individuals need a wider variety of bacteria to challenge their immune system? All of these questions are still hanging in the air without, as yet, any definitive answers, but scientific interest in the underlying role of the microbiome in inflammatory and auto-immune conditions is rapidly increasing. It's a very exciting time for probiotic research!
One thing that the study did not appear to address was the introduction of probiotic bacteria in Crohn’s sufferers, and how this may affect their populations of gut flora. With emerging research consistently suggesting that the role of the microbiome in children may affect their long-term health, this is an area that we'll be keeping a very close eye on...
Click on the links to read these other related articles:
Gut bacteria may influence autoimmunity
References
- Lewis et al (2016) Inflammation, Antibiotics, and Diet as Environmental Stressors of the Gut Microbiome in Pediatric Crohn’s Disease, Cell Host & Microbe, Volume 18, Issue 4, p489–500, 14 October 2015