

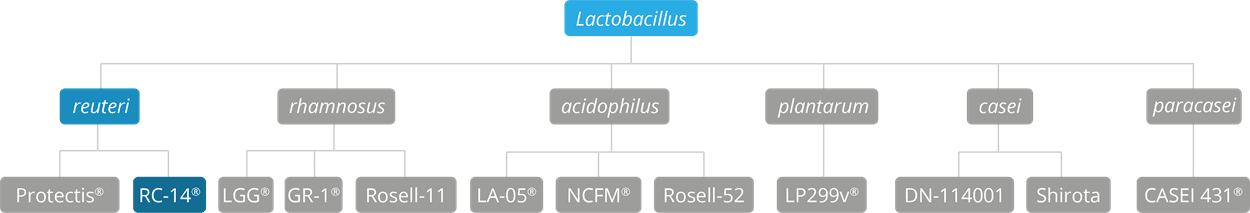
Lactobacillus reuteri RC-14® is one of the world’s most well-documented probiotic strains for women’s health, and was originally isolated from the vagina of a healthy woman. It was originally known as Lactobacillus fermentum RC-14, but has since been re-classified as Lactobacillus reuteri RC-14®. It is a member of the Lactobacillus reuteri species. Many studies and trials have used Lactobacillus reuteri RC-14® in combination with Lactobacillus rhamnosus GR-1® as both strains have been shown to colonise in the vaginal mucosa and to positively affect the composition of the vaginal microbiota. As of April 2020 L. reuteri has been officially reclassified to Limosilactobacillus reuteri and so the full strain is now also known as Limosilactobacillus reuteri RC-14® (Zheng J et al 2020).
It has been established from the results of in vitro and in vivo studies that this strain adheres to the epithelial surfaces in the uro-genital area in women (Morelli L. et al., 2004), though in vitro research suggests that it is also capable of adhering to the intestinal epithelium (Reid et al., 1993), (Velraeds et al., 1996). In doing so it replaces and displaces pathogenic bacteria, and inhibits the growth of pathogenic bacteria in both the intestine and the uro-genital area by producing lactic acid (Laughton 2006) (Burton 2003), (Cadieux 2006). Lactobacillus reuteri RC-14® also produces signalling factors that downregulate toxin production, and may have an immune modulatory activity (Lee, 2009).
Despite some limited research into its potential in other areas, the available evidence suggests that it is best recommended for genito-urinary health and, along with its sister strain Lactobacillus rhamnosus GR-1®, it is included in this database due to the sheer weight of research that has been conducted to assess its benefits for vaginal health.
N.B.: An important point to note is that, for all of the featured clinical trials which focus on the use of this probiotic strain for the support of vaginal health, all probiotic supplements were given orally rather than used topically.

Lactobacillus reuteri RC-14® has been on the worldwide market as a food supplement for many years. This historical observation permits a certain level of assumed safety, and together with clinical trial evidence it is clear that this food supplement does not pose any safety issues. A number of trials have included recording of adverse events as part of the trial design, for example Reid, G. et al., (2003). In this randomised placebo-controlled trial women took this strain in combination with Lactobacillus rhamnosus GR-1® for 60 days, a decent time frame for safety to be evaluated. There was no difference in adverse events between the probiotic and placebo groups, indicating good safety tolerance of these strains over this time period.
Survival of this strain through the gut and also to the vagina has been demonstrated clinically. This strain was recovered in faecal samples and vaginal swabs from 7 days after oral administration, indicating survival through the challenges of the gut environment and across the perineum to the vagina (Morelli, L. et al., 2004).
Clinical trials show that this strain colonises in the vagina, crowds out pathogenic yeasts and fortifies the vagina’s natural defences against Candidaalbicans. Candida albicans is the type of yeast usually implicated in vaginal yeast infections, also known as vaginal thrush.
In a clinical trial conducted to test the effects of the probiotic strains on thrush symptoms, participants with diagnosed yeast infections took an anti-fungal capsule every morning for four weeks, together with either a probiotic capsule (containing Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1®), or a placebo. At the end of the four week period, it was found that those who had been taking the probiotic experienced a significant improvement in symptoms (e.g. less vaginal discharge), and fewer yeast cells were present in their samples compared to those in the placebo group (Martinez et al., 2009).
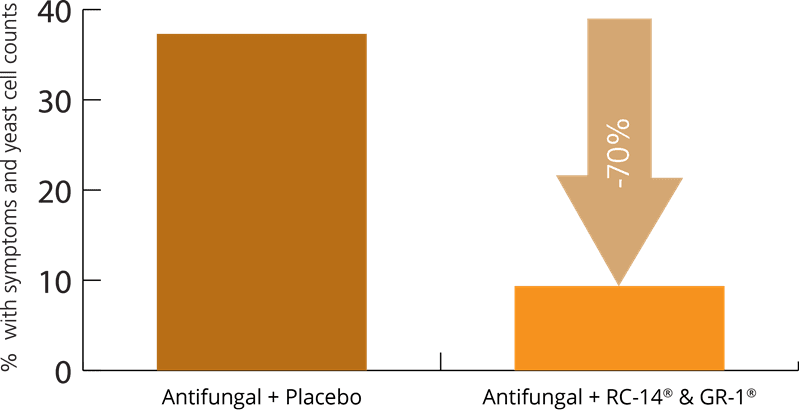
Another study involved 59 premenopausal women who had been diagnosed with chronic vulvo-vaginal candidiasis (thrush). The women were given either a probiotic containing Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1®, or a placebo, alongside conventional treatment of Fluconazole (anti-fungal medication) for three months. It was found that significantly fewer of those in the probiotic intervention group had a reoccurrence of their thrush symptoms (Anukam et al., 2009).
Bacterial vaginosis (BV) is essentially dysbiosis of the vaginal microbiota, and suggests a chronic imbalance of healthy bacteria and pathogenic bacteria. This bacterial imbalance results in the unpleasant symptoms typically experienced by sufferers of BV, which include a white-grey vaginal discharge, with a distinctive, foul-smelling "fishy" odour. Vaginal itching and burning during urination are also common symptoms.
Trials to determine the effect of Lactobacillus reuteri RC-14® on the symptoms and incidence of BV are usually conducted by using this strain in combination with Lactobacillus rhamnosus GR-1®. These strains together have been found to colonise the vagina, and like most Lactobacilli, are believed to produce substances known as biosurfactants which may help to break down the biofilm, a slimy barrier created by pathogenic bacteria which protects them and allows them to thrive (Wilson M., 2001).
In order to demonstrate this effect, a randomised, double-blind, placebo-controlled trial was set up to assess the efficacy of the bacterial strains, Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14®, in women with bacterial vaginosis who were otherwise healthy. The trial included 544 females over the age of 18 who had all been diagnosed with the vaginal infection. The subjects were randomly selected to be given their respective supplements, a placebo or the probiotic capsules, for a six week period. At week six and week twelve, the participants had vaginal swabs taken. It was found that the vaginal microbiota had normalised in just 40 (26.9%) of the women in the placebo group, compared to 243 (61.5%) of women in the probiotic group (Vujic et al., 2013).
These statistically significant results were substantiated by the results of a further clinical trial, where 62 women with bacterial vaginosis were equally divided to receive either the probiotic supplement Lactobacillus reuteri RC-14® with Lactobacillus rhamnosus GR-1®, or a placebo, at the same time as taking the antibiotic Tinidazole. In order to try and monitor changes in the bacterial microflora before and after treatment, 16S rRNA gene sequencing was used. It was found that Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1® induced an increase in the relative abundance of indigenous Lactobacilli flora in women with BV, helping restore homeostasis (Macklaim et al., 2015).
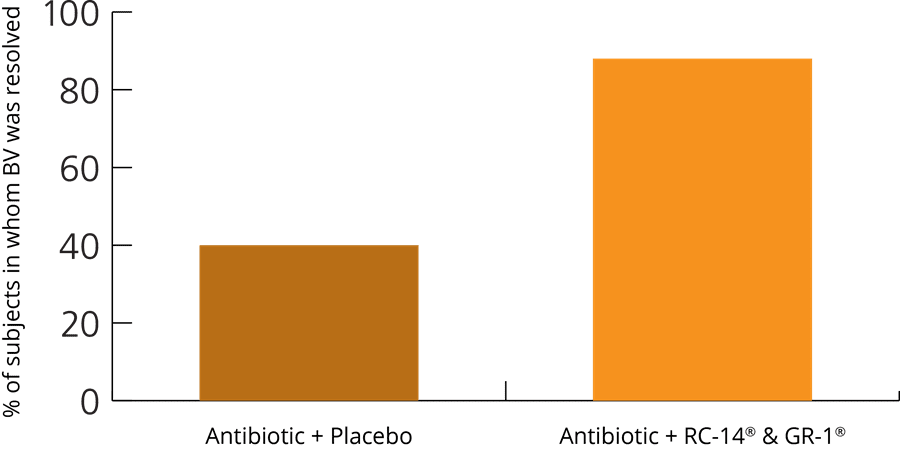
In a later study, a total of 125 women with BV were enrolled in a clinical trial to ascertain the effects of probiotics when used alongside antibiotics. The women were given a week’s course of antibiotics, and then selected to receive either a probiotic supplement containing Lactobacillus reuteri RC-14 and Lactobacillus rhamnosus GR-1®, or a placebo, alongside the medication. The women were monitored and it was found that, during the treatment week and for three weeks afterwards, the BV infection was resolved in 40% of those women who took the medication alone; however, the infection was cleared in much greater number (88%) of the women who took the probiotic with their medication (Anukam et al., 2006).
In another randomised, placebo-controlled study, 32 women with bacterial vaginosis were divided into two groups of 16. In the treatment group, the women were given a probiotic supplement containing Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1®, and in the other group, they were given a placebo. Both groups were given a 7 day course of antibiotics, and then alongside this medication, were also given two supplement capsules (either probiotic or placebo) for the duration of the antibiotic treatment. Following the cessation of antibiotic treatment, the supplements continued to be administered at a dose of two capsules per day for a further three weeks. This dose was then reduced to one capsule per day and administered for a further month, in order to try and assess whether the probiotics were able to maintain a healthy genital microflora throughout the treatment period.
The results revealed that 13 (81%) of the women in the probiotic group had a normal vaginal status and pH within 30 days of taking the probiotic, compared to just 5 (31.3%) in the placebo group. A follow-up confirmed that the results were still maintained after sixty days (Shamshu R. et al., 2017).
Further relevant studies: Anukam et al., (2006), Burton et al., (2003), Cianci et al., (2008), Hummelen et al., (2010), Kamala et al., (2009), Krauss-Silva et al., (2011), Martinez et al., (2009), Petricevic et al., (2008), Perisić et al., (2011), Reid et al., (2001), Reid et al., (2001), Reid et al., (2003), Reid et al., (2003), Reid et al., (2004), Thulkar et al., (2010).
In the same way as it has been used in studies concerned with the support and resolution of bacterial vaginosis, Lactobacillus reuteri RC-14® has often been studied in combination with Lactobacillus rhamnosus GR-1® in trials focusing on cystitis, or Urinary Tract Infections (UTIs). It is thought that these strains together help to alleviate and protect against UTIs due to the bacteriocins, lactic acid, and hydrogen peroxide they produce, which help to discourage and inhibit the survival of the pathogens that commonly cause cystitis, such as Escherichia coli.
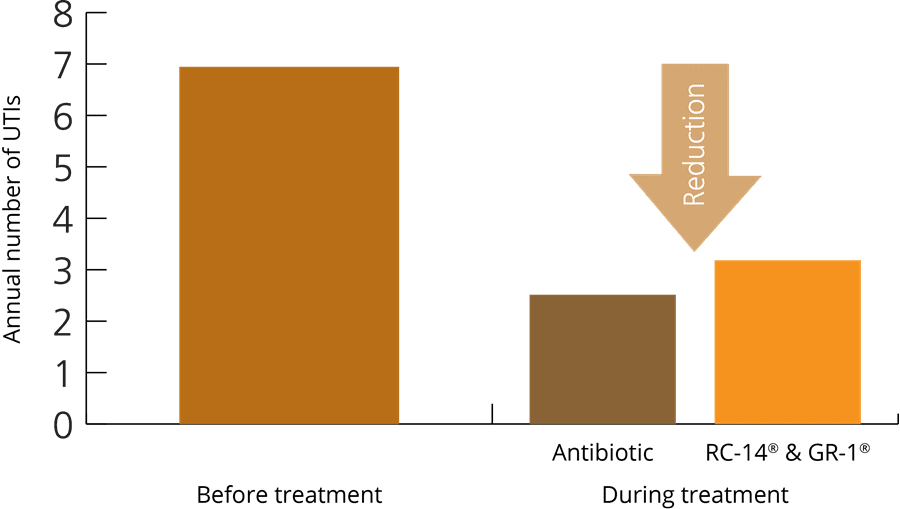
In one large trial involving 252 post-menopausal women who were suffering from recurrent UTIs, the women were given either a supplement containing the probiotic combination of Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1®, or long-term antibiotics (trimethoprim-sulfamethoxazole), for a period of one year. After twelve months, it was found that the occurrence of UTIs had been reduced by 50%, the same in both groups; however, it was also found that after one month, 90% antibiotic resistance had taken place in the antibiotic group. This results of this trial were extremely significant, as they indicated that a natural food supplement (probiotic) could perform as effectively as antibiotic medication, but without the risk of the pathogens becoming resistant - see graph above (Beerepoot et al., 2012).
Further relevant studies: Bruce, A.W. et al.,(1988), Bruce A.W. et al., (1992), Karlsson M. et al., (2012), Reid et al., (1988). Reid et al., (1995),
The presence of Group B streptococcus (GBS) is often identified during pregnancy. It is considered to be a normal resident of the gut flora in 20-30% of people (both men and women), and it is believed to ‘colonise’ the vagina in roughly 22% of all women. Carrying this type of bacterium is not generally associated with any health risks or symptoms, and most pregnant women who are known to host group B streptococcus (GBS) bacteria go on to have healthy babies; however, there's a small risk that GBS can pass to the baby during childbirth. Rarely, GBS infections in new-born babies can cause complications so if doctors believe that there is a risk of infection to a new baby, then they may prescribe antibiotics for mother and/or the child.
A randomised placebo-controlled trial was conducted to try and ascertain the effect of Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14® on 110 pregnant women who had tested positive for GBS. During the trial, the women were randomly assigned to be part of either a probiotic treatment group, or the control group, and in total, 99 of the women completed the study. Those in the treatment group were all given a supplement containing the probiotic combination, and those in the control group were given a placebo supplement. It was found that the GBS colonisation changed from positive to negative in 42.9% of the probiotic group, while just 18% of those in the placebo group experienced this positive shift. The authors concluded that these two strains of probiotic bacteria may reduce the vaginal and rectal rate of colonisation of GBS in pregnant women (Ho et al., 2016).
Further relevant studies: Kamala et al. (2009), Krauss-Silva et al., (2011).
Inflammation is a normal and essential part of the immune system response, occurring when foreign substances or bacteria enter the body, or when there is trauma to a body part. However, associated health issues occur when these inflammatory responses are prolonged and misdirected to benign substances, or the body’s own tissues. The role of probiotics to help modulate inflammatory responses is a developing area of probiotic research.
The combination of Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1® were tested to assess the anti-inflammatory potential of probiotics in patients who were suffering from Inflammatory Bowel Disease (IBD). For the purposes of the trial, 20 healthy controls were sought, to compare with 20 patients who were suffering from IBD; fifteen of the IBD group were suffering from Crohn’s disease, and five were suffering from ulcerative colitis. All of the subjects were given a yoghurt containing the probiotic combination each day for a period of one month. An increase in the presence of T cells was observed in those who were taking the probiotic. The formation of a desirable anti-inflammatory environment in the peripheral blood of these IBD patients was also noted, with fewer such effects being observed in the healthy control group.
The positive effects associated with consumption of the probiotic yoghurt were confirmed by a follow-up study, in which subjects consumed plain, non-probiotic yoghurt but did not experience the same benefits. These results indicate that the anti-inflammatory effects noted in the original study were associated with the presence of the Lactobacillus probiotic strains GR-1® and RC-14® (Baroja, 2007).
Other relevant studies: de los Angeles Pineda M.et al., (2011).
Authors: Information on this strain was gathered by Joanna Scott-Lutyens BA (hons), DipION, Nutritional Therapist; and Kerry Beeson, BSc (Nut.Med) Nutritional Therapist.
Last updated - 7th May, 2020
As some properties & benefits of probiotics may be strain-specific, this database provides even more detailed information at strain level. Read more about the strains that we have included from this genus below.
Lactobacillus acidophilus strains: Lactobacillus acidophilus LA-05, Lactobacillus acidophilus NCFM®, Lactobacillus acidophilus Rosell-52.
Lactobacillus casei strains: Lactobacillus casei Shirota, Lactobacillus casei DN-114001.
Lactobacillus plantarum strains: Lactobacillus plantarum LP299v.
Lactobacillus reuteri strains: Lactobacillus reuteri Protectis.
Lactobacillus rhamnosus strains: Lactobacillus rhamnosus LGG®, Lactobacillus rhamnosus HN001, Lactobacillus rhamnosus GR-1® and Lactobacillus rhamnosus Rosell-11.
Lactobacillus paracasei strains: Lactobacillus paracasei CASEI 431®.
For more information and the latest updates on probiotics, please visit Probiotic Professionals pages.
Anukam K.C. et al., (2006), ‘Augmentation of antimicrobial met*******ole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial’. Microbes Infect. 8(6): 1450-4.
Anukam K.C. et al., (2006), ‘Clinical study comparing probiotic Lactobacillus GR-1 and RC-14 with met*******ole vaginal gel to treat symptomatic bacterial vaginosis’ Microbes Infect; 8(12-13: 2772-6.
Anukam KC. et al., (2009), ‘Oral use of probiotics as an adjunctive therapy to fluconazole in the treatment of yeast vaginitis: A study of Nigerian women in an outdoor clinic’. Microb Ecol. Health Dis., 21(2): 72-77.
Baroja M. et al., (2007), ‘Anti-inflammatory effects of probiotic yogurt in inflammatory bowel disease patients’ Clin Exp Immunol., 149(3):470-9.
Beerepoot et al., (2012), ‘Lactobacilli vs antibiotics to prevent urinary tract infections: a randomized, double-blind, non-inferiority trial in postmenopausal women’. Arch Intern Med., 172(9):704-12.
Bisanz J.E. et al., (2014), ‘A systems biology approach investigating the effect of probiotics on the vaginal microbiome and host responses in a double blind, placebo-controlled clinical trial of post-menopausal women’. PLoS One, 9(8):e104511.
Burton et al., (2003), ‘Improved Understanding of the Bacterial Vaginal Microbiota of Women before and after Probiotic Instillation’. Appl. Environ. Microbiol., 69(1):7-101.
Cadieux P., (2006), ‘Identification of anti-infective signals from lactobacilli’. Ph. D Thesis, University of Western Ontario, Canada.
Cianci et al., (2008), ‘Efficacy of Lactobacillus rhamnosus GR-1 and of Lactobacillus reuteri RC-14 in the, treatment and prevention of vaginosis and bacterial vaginitis relapses’ Minerva Ginecol., 60(5):369-76.
de los Angeles Pineda M. et al., (2011), ‘A randomized, double-blinded, placebo-controlled pilot study of probiotics in active rheumatoid arthritis’. Med Sci. Monit., 17(6):CR347–CR354.
Gardiner E. et al., (2002), ‘Oral administration of the probiotic combination Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 for human intestinal applications’. International Dairy Journal, 12(2-3):191–196.
Gardiner G. et al., (2002), ‘Persistence of Lactobacillus fermentum RC-14 and Lactobacillus rhamnosus GR-1 but Not L. rhamnosus GG in the Human Vagina as Demonstrated by Randomly Amplified Polymorphic DNA’. Clin Vaccine Immunol., 9(1):92-96.
Hummelen et al., (2010), ‘Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 to prevent or cure bacterial vaginosis among women with HIV’. Int.J. Gynaecol. Obstet., 111(3):245-8.
Hummelen et al., (2011), ‘Effect of 25 weeks probiotic supplementation on immune function of HIV patients’. Gut microbes, 2(2): 80-85.
Ho M. et al., (2016), ‘Oral Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 to reduce Group B Streptococcus colonization in pregnant women: A randomized controlled trial’. Taiwanese Journal of Obstetrics & Gynaecology, 55(4):515-8.
Kamala et al., (2009), ‘Benefits of probiotic treatment in cases of bad obstetric history (BOH) and for prevention of post IVF pregnancy complications’. J. Obstet. Gynecol India; 59(4):336-339.
Krauss-Silva et al., (2011), ‘A randomised controlled trial of probiotics for the prevention of spontaneous preterm delivery associated with bacterial vaginosis: preliminary results’. Trials, 8(12):239.
Laughton J.M. et al., (2006), ‘Inhibition of expression of a staphylococcal superantigen-like protein by a soluble factor from Lactobacillus reuteri’. Microbiology, 152(4):1155-67.
Lee Y. & Salminen S., (2009), Handbook of Probiotics and Prebiotics. 2e, Hoboken: John Wiley & Sons.
Macklaim et al., (2015), ‘Changes in vaginal microbiota following antimicrobial and probiotic therapy’. Microbial Ecology in Health and Disease, 26:27799.
Martinez et al., (2009), ‘Improved treatment of vulvovaginal candidiasis with fluconazole plus probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14’. Lett Appl Microbio., 48(3):269-74.
Martinez et al., (2009), ‘Improved cure of bacterial vaginosis with single dose of tinidazole (2 g), Lactobacillus rhamnosus GR-1, and Lactobacillus reuteri RC-14: a randomized, double-blind, placebo-controlled trial’. Can. J. Microbiol., 55(2):133-8.
Morelli L. et al., (2004), ‘Utilization of the intestinal tract as a delivery system for urogenital probiotics’ J Clin Gastroenterol., 38(6S):S107-10.
Perisić et al., (2011), ‘The influence of probiotics on the cervical malignancy diagnostics quality’. Vojnosanit Pregl., 68(11):956-60.
Petricevic et al., (2008), ‘Randomized, double-blind, placebo-controlled study of oral lactobacilli to improve the vaginal flora of postmenopausal women’. Eur. J. Obstet. Gynecol. Reprod. Bio.,141(1):54-7.
Reid G. et al., (1993), ’Adhesion of three Lactobacillus strains to human urinary and intestinal epithelial cells’. Microbios., 75(302):57-65.
Reid G. et al., (2017), ‘The development of probiotics for women’s health (review)’. Canadian Journal of Microbiology, 63:269–277.
Reid et al., (2002), ‘Ability of Lactobacillus GR-1 and RC-14 to stimulate host defences and reduce gut translocation and infectivity of Salmonella typhimurium’. Nutraceeut. Food, 7:168-173.
Reid et al., (2004), ‘Nucleic acid-based diagnosis of bacterial vaginosis and improved management using probiotic lactobacilli’. J. Med. Food., 7(2):223-8.
Reid et al., (2003), ‘Oral use of Lactobacillus rhamnosus GR-1 and L. fermentum RC-14 significantly alters vaginal flora: randomized, placebo-controlled trial in 64 healthy women’. FEMS Immunol. Med. Microbiol., 35(2):131-4. (N.B.: L. fermentum RC-14 has since been re-classified as L. reuteri RC-14).
Reid et al., (2003), ’Effect of lactobacilli oral supplement on the vaginal microflora of antibiotic treated patients: Randomized, placebo-controlled study’. Nutraceut. Food, 8:145-8.
Reid et al., (2001), ‘Oral probiotics can resolve urogenital infections’. FEMS Immunol. Med. Microbiol. 30(1):49-52.
Reid et al., (2001), ‘Probiotic Lactobacillus dose required to restore and maintain a normal vaginal flora’. FEMS Immunol. Med. Microbiol. 32(1):37-41.
Shamshu, R., et al., (2017), ‘Role of probiotics in lower reproductive tract infection in women of age group 18 to 45 years’. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 6(2):671-681.
Thulkar et al., (2010), ‘Probiotic and met*******ole treatment for recurrent bacterial vaginosis’, Int. J. Gynaecol. Obstet., 108(3):251-2.
Velraeds M. et al., (1996), ‘Inhibition of initial adhesion of uropathogenic Enterococcus faecalis by biosurfactants from Lactobacillus isolates’. Appl, Environ, Microbiol. 62(6):1958-1963.
Vujic et al., (2013), ‘Efficacy of orally applied probiotic capsules for bacterial vaginosis and other vaginal infections: a double-blind, randomized, placebo-controlled study’. Eur. J. Obstet. Gynecol. Reprod. Biol., 168(1):75-9.
Wilson M., (2001), ‘Bacterial biofilms and human disease’. Science progress, 84:235-54.
Zheng J, Wittouck S. et al., (2020) 'A taxonmonic note on the genus Lactobacillus: Description of 23 novel genera, emended description of the genus Lactobacillus Beijerinck 1901, and union of Lactobacillaceae and Leuconostocaceae'. Int.J.Syst.Evol.Microbiol, 70(4): 2782-2858. DOI: 10.1099/ijsem.0.004107